Simplicity. Transparency. Versatility.
Creating unrivaled connections
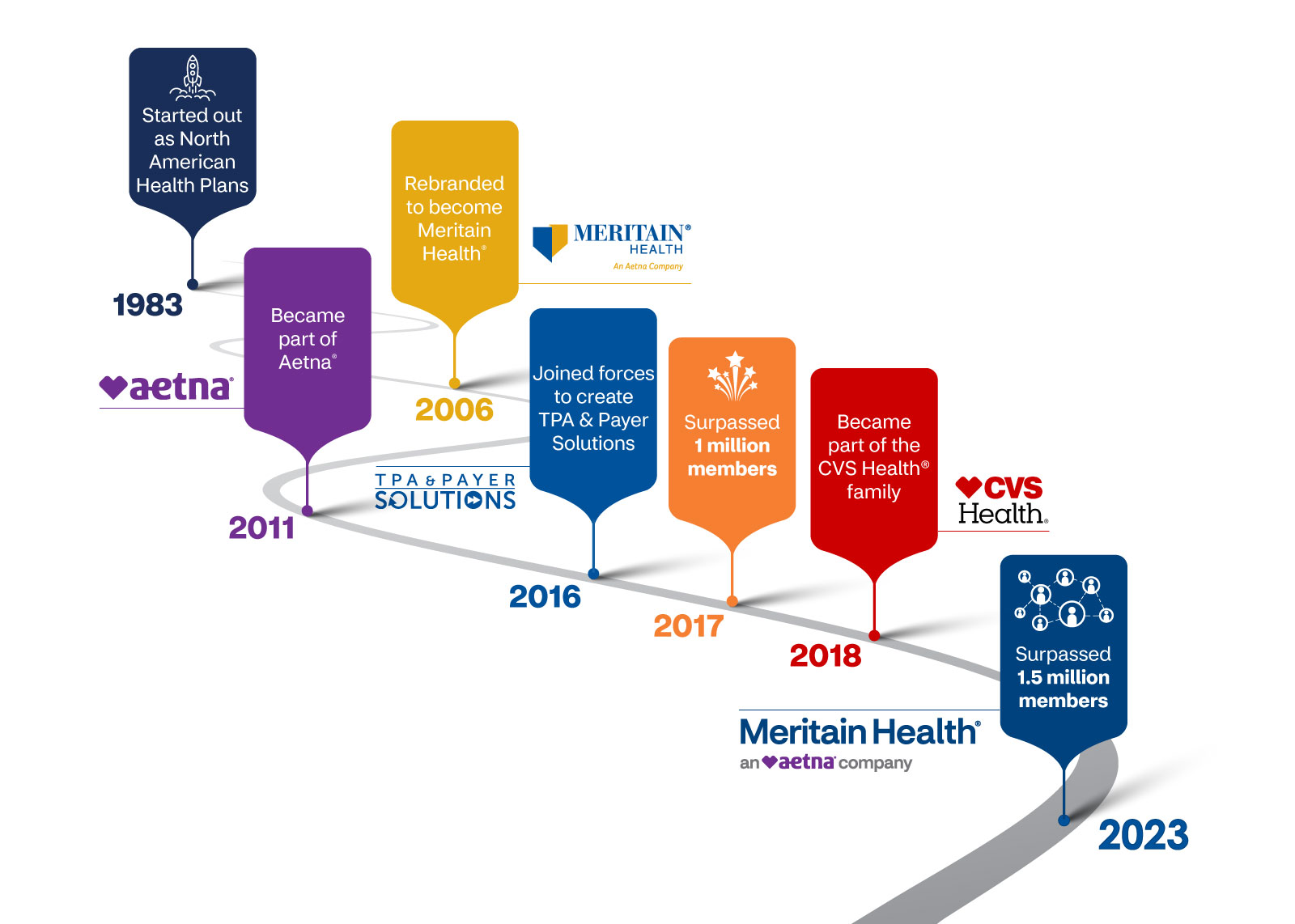
Meritain Health® is committed to optimizing your health benefits. We take pride in being one of the nation’s largest third party administrators (TPAs), and a subsidiary of Aetna® and Fortune 6 company CVS Health®.
Our backstory
For 40 years, we’ve offered self-funded health care benefits administration for plan sponsors and health plans nationwide. We combine the strength of a national carrier, versatility of a TPA, and the ability to create benefit plans as unique as our customers. Plus, we have the ability to introduce progressive, seamless solutions through our TPA-of-choice partnerships with leading navigation companies and captive arrangements. Meritain Health is ready to meet your common—and not so common—self-funding challenges.
And, by creating one-of-a-kind access and affordability, we’re proud to now support 1.5 million members nationwide. With access to over 1.6 million health care providers, competitive network discounts, leading point solutions and modern pharmacy plans, our plan sponsors and members enjoy quality care how they want to receive it, without sacrificing savings.
With simplicity, transparency and versatility—we’ll make your health benefit goals a reality.
How can we help you?
Member Services
For quickest service, dial the toll-free number on the back of your ID card.
Provider Services
For 24-hour automated phone benefits and claims information, call us at 1.800.566.9311.
Privacy, Security and Legal
